News
Antibiotic resistance in livestock animals is stabilizing
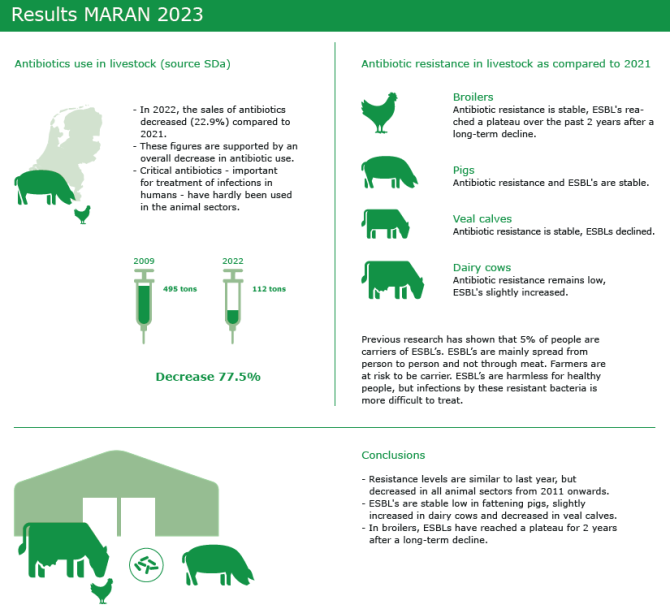
As the sales of antimicrobial veterinary medicinal products in the Netherlands declined over the years since 2009, so did the antimicrobial resistance in animals. This declining trend of antibiotic resistance in animals has stabilised for most antibiotics, according to the data presented in the MARAN report, an annual update of antibiotic resistance in animals.
Antibiotics are used in animal husbandry to treat bacterial infections. Bacteria can become resistant to antibiotics for which overuse and improper use are contributing factors, therefore antibiotic stewardship is important. Wageningen Bioveterinary Research (WBVR) studies the occurrence, spread and prevention of antimicrobial resistance (AMR) in bacteria obtained from livestock. WBVR is leading partner in the yearly MARAN report, which gives an update on the status of antimicrobial resistance in animals in the Netherlands. The monitoring of AMR in food-producing animals and food is essential to provide reliable information on the development and spread of antibiotic resistance.
Compared to previous years the reduction in antibiotic resistance was less pronounced in 2022
“As in previous years, the year 2022 again showed a further reduction in the sales and use of antimicrobial veterinary medicinal products. This trend was accompanied by a decrease in antimicrobial resistance. However, compared to previous years this reduction was less pronounced and in some cases absent,” says WBVR-researcher Kees Veldman, head of the National Reference Laboratory on antimicrobial resistance in animals and key editor of the MARAN report.
Monitoring of antibiotic resistance
Monitoring of trends in antibiotic resistance in livestock and food is determined by analysing the results generated within an annual standard monitoring program. In practise, this means that bacterial cultures of faecal samples (or meat samples) are made. The next step is antimicrobial susceptibility testing of indicator bacteria such as E. coli as well as zoonotic bacteria such as Salmonella and Campylobacter. This is done using standardised antibiotic panels according to EU legislation. In addition, the collected samples are screened for the presence of bacteria with specific types of resistance that are considered a risk to human health. This includes E. coli exhibiting resistance to 3rd and 4th generation cephalosporins (ESBLs) or resistance to carbapenem antibiotics (CPE).
The substantial decline in antibiotic use in animals since 2009 is reflected by a trend of decreasing resistance in indicator bacteria, followed by levelling off in more recent years. This effect of decreasing resistance is less clear in zoonotic bacteria like Salmonella and Campylobacter. Furthermore, the prevalence of ESBLs remained low in most animal sectors. As in previous years, no CPE was detected in 2022.
Whole genome sequencing
Until recently, the resistance pattern of ESBL-producing E. coli was measured with a phenotypic susceptibility test. In the past two years, this has been replaced by whole genome sequencing. Research shows that the genetic analysis provides the same information as the susceptibility tests. In addition, whole genome sequencing provides much more information, such as relationships between bacteria. This type of information supports knowledge about the potential spread of resistant bacterial clones.
Infographic
View the infographic below about antibiotic resistance in livestock animals.
NethMap: antibiotic resistance in humans
Figures on antibiotic use and resistance in humans are annually reported in NethMap and jointly published with MARAN. NethMap shows that the antibiotic use in hospitals was about the same as in the years before the COVID pandemic. GPs prescribed antibiotics slightly less often. Furthermore, hospitals and nursing homes reported more outbreaks of infections due to resistant bacteria than in the COVID years. This number is still lower than in the years before the pandemic.
Despite the stable antibiotic resistance in humans, attention to resistant bacteria remains necessary. People who have been hospitalized abroad in particular can carry bacteria that are resistant to multiple types of antibiotics at the same time. Washing hands and other – personal - hygiene measures remain necessary to prevent these bacteria from spreading. It is also important to prevent unnecessary and incorrect use of antibiotics as much as possible.